Applying artificial intelligence (AI) in the nodal metastasis microenvironment may enhance accuracy in predicting extracapsular nodal extension (ECE) for oropharyngeal carcinoma patients, as revealed in a poster at the 2024 Symposium on Multidisciplinary Head and Neck Cancers by the American Society for Radiation Oncology (ASTRO).
Utilizing support vector machine (SVM) with linear discriminant analysis (LDA), incorporating 24 radiomics features while eliminating correlated ones, achieved a 75.5% accuracy (0.76 area under the curve [AUC]) in ECE detection. Moreover, SVM/LDA demonstrated a 72.6% accuracy (0.61 AUC, 0.41) when utilizing 10 topological features. The accuracy improved to 81.1% (0.8 AUC) by combining both radiomic and topological features in the analysis.
Applying support vector machine (SVM) with linear discriminant analysis (LDA), utilizing 51 radiomics features and eliminating correlated ones, achieved an 84.9% accuracy (0.87 area under the curve [AUC]) in ECE detection. The combination of SVM and LDA using 33 topographical data analysis (TDA) features yielded an accuracy of 80.2% (0.79 AUC). The integration of both radiomics and TDA features in the analysis significantly enhanced the accuracy of ECE detection to 90.6% (0.93 AUC).
Upon incorporating human papillomavirus (HPV) status into the multi-machine learning model, researchers observed an elevated accuracy of 92.5% (AUC, 0.95). This approach yielded a true-positive rate of 100% and a true-negative rate of 90%.
Applying artificial intelligence for the analysis of the nodal metastasis microenvironment enhances the accuracy of predicting extracapsular extension (ECE) in patients with oropharyngeal cancer,” commented Dr. Annie W. Chan, an oncologist and radiation oncologist. She holds positions as the Director of the Head and Neck Radiation Oncology Research Program and the Head and Neck Service at Massachusetts General Hospital. The authors underscored the importance of validating these findings with datasets from multiple institutions.
The authors highlighted that the approach of reducing treatment intensity for individuals with early-stage oropharyngeal carcinoma typically includes performing surgery with or without adjuvant radiotherapy, while excluding concurrent chemotherapy. However, the identification of nodal extracapsular extension (ECE) through pathology indicated the need for postoperative chemotherapy in this specific group.
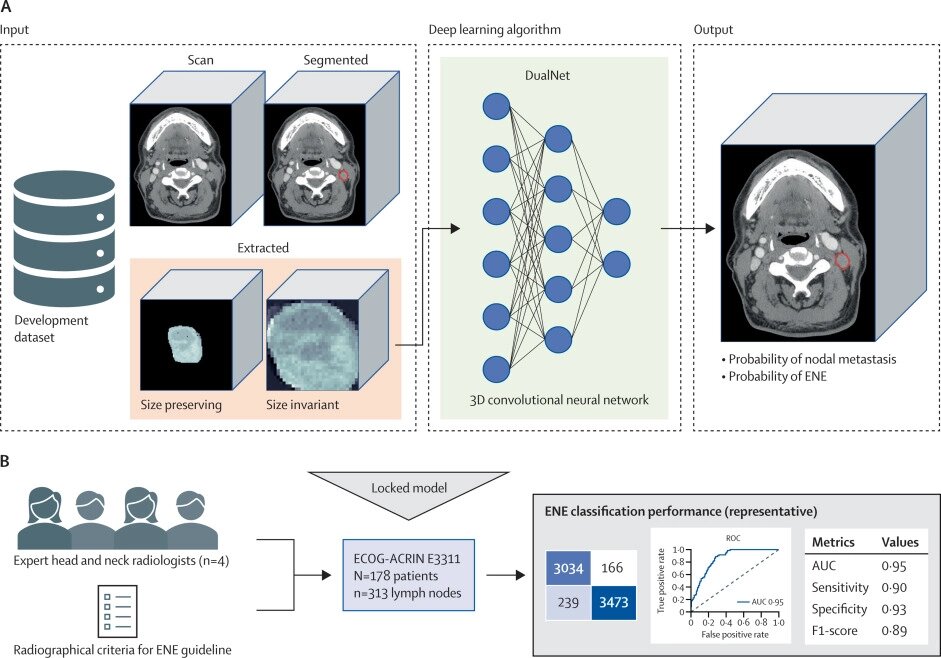
In a decision-making system guided by radiologists, the evaluation of extracapsular extension (ECE) in patients involved CT imaging followed by visual assessment by radiologists, influencing subsequent treatment decisions. Individuals with ECE-positive disease underwent a combination of radiation and chemotherapy, while those with ECE-negative disease opted for either transoral surgery or neck dissection. Subsequently, patients with consistently ECE-negative findings proceeded with radiotherapy, while those diagnosed with ECE-positive disease were directed toward a treatment approach involving both radiation and chemotherapy.
The researchers found that utilizing clinical annotations or CT imaging with machine learning and deep learning algorithms to predict extracapsular extension (ECE) yielded AUCs ranging from 0.58 to 0.85, a performance level they deemed suboptimal.
The investigators suggested that both involved nodes and the peritumoral environment in patients with oropharyngeal cancer collectively played a role in determining the presence of ECE. They conducted a study to assess whether employing AI-based tools in the microenvironment of nodal metastases could enhance their ability to predict ECE.
In total, 171 patients diagnosed with newly resectable oropharyngeal carcinoma underwent upfront transoral robotic surgery and neck dissection at Massachusetts General Hospital and Massachusetts Eye and Ear Infirmary between 2016 and 2022. Preoperative high-resolution CT scans were conducted for each patient, and experienced head and neck radiologists determined the absence of extracapsular extension (ECE). Furthermore, the pathology of surgical specimens, including the presence and extent of ECE, was assessed by a head and neck pathologist.
The investigators characterized the perinodal microenvironment as the stromal tissues surrounding the nodes as identified through preoperative CT imaging. Radiomics and topological features were also extracted from the nodal and perinodal microenvironment to create predictions for detecting ECE.