Exclusive Article at EMRIndustry by Thanh Tran, CEO of Zoeticx
Thanh Tran is CEO of Zoeticx, Inc., a medical software company located in San Jose, CA. He is a 20 year veteran of Silicon Valley’s IT industry and has held executive positions at many leading software companies.
A new Black Book survey finds that 90% of hospitals and 94% of independent physicians don’t trust the business model of public HIEs and have concerns over how much of the cost payers will be fronting, causing a contraction in the HIE market. Meanwhile the ONC and medical industry are at odds on how to address the interoperability issue. The ONC does not even mention middleware in any of its plans.
Even HL7 does not provide the seamless connection of middleware and is only capable of connecting one medical facility to another and requiring specific end point interfaces to even do that. For every additional facility, a customized interface must be built. At the end of the day, HL7 is really a point-to-point customized interface requiring extra steps. A middleware platform does not tie developers to specific hospitals or EHRs and allows universal access.
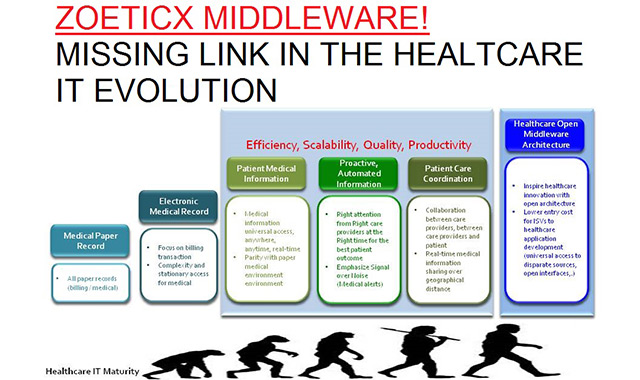
But some healthcare 2.0 innovators such as Zoeticx are offering middleware solutions that have proven themselves in other industries. Vertical markets such as retail, banking, transportation, and others have long ago solved interoperability with middleware solutions.
Middleware is the technology to drive change, innovation and disruptive transformation to solve EHR interoperability challenges. Patient’s lives can depend on it and in some cases their lives will depend on it. It will help bring to an end the more than 1,000 patients who die daily from preventable medical errors. Middleware should be the standard operating system for EHRs to finally bring lack of interoperability to an end without the risk of HIEs. The medical community has so far not provided a better solution to a problem that can be addressed today.
“Middleware should be the heart of an EHR’s operating system. It will enable medical institutions to seamlessly connect multiple EMRs, resulting in a convenient, consistent and universal view of patient records from a single platform, regardless of where they reside,” says Tiffany Casper, CEO of EMR Consultants, Inc. She implements EHR systems for medical facilities.
“A middleware architecture has been shown to be the best technological solution for addressing the problem of EHR interoperability. The middleware platform facilitates the transparent, yet secure, access of patient health data, directly from the various databases where it is stored. A server-based middleware framework supporting access to the various patient health data stores allows for a scalable, unified and standardized platform for applications to be developed upon.
The middleware architectural design has been successfully used to link data from multiple databases, irrespective to the database platform or where the database is located,” says Donald M. Voltz, MD, Department of Anesthesiology and Medical Director of the Main Operating Room at Aultman Hospital in Canton, OH. He is also board certified in Informatics and is an Assistant Professor of Anesthesiology at Case Western Reserve University and Northeast Ohio Medical University.
Top Ten Reasons for EHR’s to Use Middleware for Connectivity
- Application Developers Can Focus on Healthcare Apps—Enables medical record app developers to focus on their healthcare solution by freeing them from dealing with a diverse, complex EHR infrastructure.
- Inspires the Next Generation of Healthcare Innovative Solutions—These solutions are inspired by expanding the market for the next generation of healthcare applications rather than being tied down to a stack approach, depending on the particular EHR vendor.
- Improves Patient Care Outcomes—Patients will receive better healthcare outcomes when application developers can inspire more Patients will also benefit from the next generation of applications as they will address providers’ specific needs in diverse operational care environments.
- Saves Healthcare IT Dollars—Focuses the healthcare IT budget on addressing providers’ needs instead of building and re-building the patient record infrastructure.
- Proven Technology—A proven technology used for decades in many industries such as financial, retail, manufacturing and other markets.
- Easy Integration—Enables healthcare integration with diverse, deployed legacy systems, including EHR systems. It addresses EHR interoperability as part of overall integration challenges.
- Passive to Active Healthcare IT Environment—It turns passive healthcare IT environments into active ones to enhance communication and collaboration among care providers.
- Avoids Data Duplication—Cost efficient, simplified administration. Offers a better privacy protection solution than HIEs by addressing EHR interoperability while fulfilling the demand to support the patient care continuum in an operational care environment.
- Eliminates Wastefulness—Addressing healthcare IT integration is much more cost efficient than the “Rip-and-Replace” approach.
- Extends EHR Usefulness—Protects and extends healthcare IT investments in EHR and EMR systems.