By Dr. Donald Voltz, MD, Aultman Hospital, Department of Anesthesiology, Medical Director of the Main Operating Room, Assistant Professor of Anesthesiology, Case Western Reserve University and Northeast Ohio Medical University.
A board-certified anesthesiologist, researcher, medical educator, and entrepreneur. With more than 15 years of experience in healthcare, Dr. Voltz has been involved with many facets of medicine. He has performed basic science and clinical research and has experience in the translation of ideas into viable medical systems and devices.
Thanh Tran, CEO of Zoeticx, Inc. also contributed.
Dr. Voltz and Than Tran will be making a presenting the topic of “Proactive and Actionable Information Flow and Its Positive Impact on Risk Management”, Thursday, August 14, 11:45-12:15 Room 192A at the Allscripts Client Experience, August 12-15, McCormick Place, Chicago. Visit them at Booth ADP-32.
If a recent New York Times/Reuters article, New Form of U.S. Healthcare Saves Money, Improves Quality, One Insurer Finds , CareFirst BlueCross BlueShield announced their medical home saved $130 million dollars over care delivered in a standard fee-for-service model. One of the significant points made in this article was that a key element of the medical home model is data.
Some of the information required to take care of patients in a cost-conscious manner includes patient and disease specific data, information about which specialists are especially pricey, as well as meta data generated from intelligent systems such as electronic medical records. These records alert doctors to overdue check-ups, abnormal laboratory values, medication renewals, and adverse drug interactions. They also call attention to chronic conditions, including asthma and diabetes, in an attempt to optimize costs and long term patient outcomes.
Healthcare, like many other business sectors, is dependent on data for decisions and treatment plans. Medicine has always depended on data, be it from a patients history, physical examination, laboratory studies or other tests. When a single physician oversaw an entire patient’s care, items that needed to be addressed were done by this physician and other providers such as nurses knew who to contact with questions and issues to be addressed.
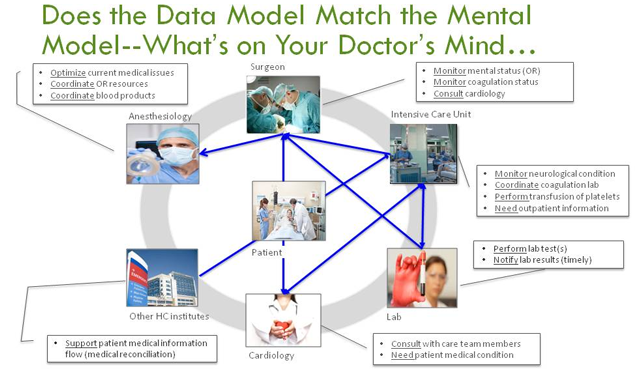
Care is no longer managed by a single provider, but instead by a care team and across a care continuum. In this distributed care environment, it is important to ensure all collected patient information is reviewed, addressed, and the net phase documented to keep all involved providers up to date on the management of care.
The simple act of ordering a set of labs can result in issues that have no defined accountability for the management of the results. It is well assumed that the ordering provider is the one who is responsible for reviewing and addressing the results in a timely manner, however, others on the care team might be expected to address any abnormalities or to order additional tests based on the result.
We have not yet established ways to communicate and document the roles and responsibilities of care teams outside of face to face communication of patient status and review of care provided over a given time period. This face to face process is well known as rounding on patients and is the core of academic medicine. But even in academia, documentation and clarification of who will review a given order or status change in a patient is not clear.
EMR’s, although with a capability to log who has accessed a patient’s medical record, does not provide other providers with who was notified, and how a given issue or lab value was addressed. This is one area of automation where the EMR can help care coordination, provided all members of the team are connected to a given patient and notified.
Actionable Data
This “actionable data” is data that requires some type of action, be it to schedule a follow up exam such as an overdue mammogram, review and act on a laboratory/test result, patient vital signs, or change in patient status as noted by healthcare providers. Actionable data can be triggered from healthcare databases and should be presented to care providers at the right time, and in a format allowing for interpretation and intervention.
Action information provides effective management of patients by care teams and the care continuum. Future meaningful use stages will extend beyond the healthcare team to include patients. Action oriented decisions, based on medical data, will impact quality while addressing issues with the duplication of tests.
EMR’s are far superior to paper-based delivery of information, they enable enhanced workflows and data capture that address medical errors, quality, reduction in service duplication, and the sharing of information between institutions. However, user interface designs that present patient data, system requirements, and enable third-party tools to interact with healthcare databases to allow patients and physicians to access information in an actionable manner is lacking.
We have all experienced the frustration of using a poorly designed application or website. These are some of the same issues we are experiencing with current EMR implementations. The data is accessible, but not without much searching. The development of work-arounds to manage patient care and the presentation of patient information has not been optimized for those depending on the information.
Too Much Background Noise
For the most part patient healthcare data is displayed accurately, and where it is supposed to be. An additional cognitive load is placed on healthcare providers to locate, synthesize, and take action on this information and apply it to patient care. It is frustrating to navigate multiple screens, different applications, and complex tabular displays of data to locate individual data points, and connect them into the mosaic which enable decisions and diagnosis. The lack of optimized user interface design and data presentation adds much background noise that does not support a physician’s mental model and workflow of diagnosis and medical problem solving.
These issues are only part of the role of health data. Physician order entry systems and taxonomy code sets such as the soon to be required ICD-10 nomenclature are critical components to the health IT initiative. However, current technology and interface designs do not allow for efficient and consistent use of these complex tools. In many systems it is challenging to identify current orders, their activity state for a given patient, code requirements, or support for orders being placed. New tools and interfaces are required to address these deficiencies.
When defined fields are not present, or adding additional notes to clarify an order, providers utilize text-based comment fields as work-arounds in order to communicate information to others so patients can be managed in the intended way. These work-arounds might get the job done, however, it makes locating this information difficult and adds to the possibility of errors when the information is missed, something that is easy to do with this type of data entry. When a customizable workflow is not present to communicate additional patient information, the ordering of interventions or categorization and support of diagnosis and disease may not be entered into the EMR.
To overcome the limitations of the EMR, verbal orders are often given to nurses, pushing the data entry problem down the road until someone on the care team is able to find a way to enter the requisite information or possibly risk losing the information or adding a delay to information entry.
EMR Vendors are Missing the Physician’s Mental Model
Although frustrating, the concept of an EMR improving healthcare delivery through the accumulation of patient data will benefit patients, improve care and eventually make care provider’s jobs easier. Designing solutions that are in sync with the end users mental models, and how these models incorporate data in the decision making process, are starting to be appreciated in healthcare, but not from the currently EMRs.
Organizations working to create customized displays, applications that extract information from multiple EMRs or specialized healthcare data repositories are emerging into the field. Vendors offering 2.0 connectivity solutions are offering tools to assist not only clinicians in data display, but are also working to enhance communication between providers. Meanwhile they bring clarity to quality metrics and improve business decisions based on information contained in EMR systems for administrators, insurance, pharmaceutical and governmental agencies.
Healthcare 2.0 vendors are working to enhance current EMR systems to increase ROI and ease the barriers to data entry by clinicians, and to harness the power with the data being collected. Finding a way into the health care system and being welcomed by EMR vendors is a challenge that needs to be overcome to enhance and connect currently implemented systems.
Given the ONC’s interoperability vision, this is an area more physicians are becoming involved with in order to provide high quality care to their patients. Having systems in place that support physicians workflow and integrate with their mental model of healthcare delivery and disease management is the next phase of health IT. We cannot expect the entire foundations of healthcare, the diagnosis and management if disease, to have to change to meet the constraints of a technology. Instead we need to understand the needs and work to mold the technology in innovative ways to meet the demands and requirement of our healthcare system to in a meaningful and consistent way.
Meaningful Use Means Bridging Databases
We must be aware that healthcare data is equally important to patients as it is for their healthcare providers to empower them to share in the optimization of health, prevention of disease and management of acute and chronic conditions. We are sitting on the edge of Meaningful Use – Stage 3, frameworks such as those developed by Zoeticx that are able to bridge and integrate data stored in healthcare databases and present it as meaningful information to patients will assist in shared decision making with providers, allow for engagement with health, treatment planning, follow up care and improved compliance. The power comes from tools that connect disparate data so that it no longer matters where a patient’s healthcare is occurring or at what point in the care continuum for complex, multiphase treatment of disease. Data that can be connected and turned into actionable items for patients, providers, population health systems and payers is what we are all looking for in an enhanced and efficient healthcare system.
Even though the final conclusion on the benefits of the medical home delivery model has not been fully clarified, the collection and use of patient data is a key to care delivery. For the power to be realized, data has to be readily accessible, presented in a way to improve decisions, standardize treatment, reduce risks to patients, communicate across institutions and educate patients on their choices and expectations.