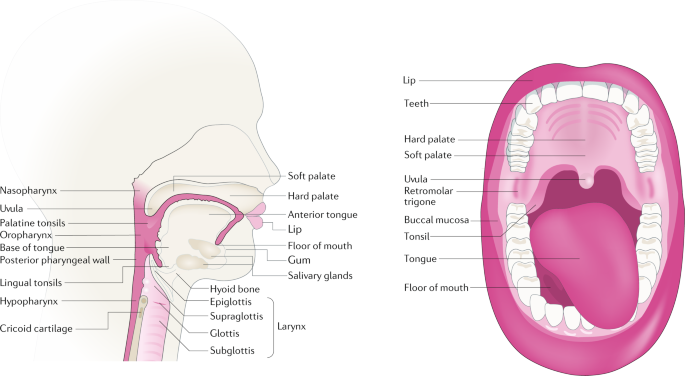
In patients with pT1-2N0 oral tongue squamous cell carcinoma undergoing partial glossectomy and elective neck dissection, inferior locoregional control (LRC) was associated with depth of invasion, lymphovascular space invasion, and positive glossectomy specimen margins. These retrospective findings, presented at the 2024 ASTRO Multidisciplinary Head and Neck Cancers Symposium, remained significant even in cases with final negative tumor bed margins.At a median follow-up of 45.6 months, the all-comer patient population exhibited 3-year locoregional control (LRC) and overall survival (OS) rates of 88.0% and 92.5%, respectively. Among patients with pT1 disease, these rates were 92.0% and 95.2%, while in those with pT2 disease, the rates were 85.0% and 90.5%.
However, during the multivariate analysis, individuals with positive glossectomy margins exhibited poorer locoregional control (HR, 6.66; 95% CI, 1.60-27.78; P = .009). Lymphovascular space invasion (HR, 6.90; 95% CI, 1.42-33.65; P = .02) and depth of invasion (HR, 1.31; 95% CI, 1.06-1.63; P = .01) were also correlated with diminished locoregional control.
The lead study author, Michael Modzelewski, MD, along with the co-investigators, stated in a poster presented at the meeting, “Patients with these risk factors may be considered for adjuvant radiotherapy to optimize disease control.”
Individuals with early-stage tongue squamous cell carcinoma typically do not undergo adjuvant radiation due to their low recurrence risk. After surgery, the status of the primary glossectomy specimen margin has been observed to have a stronger correlation with local recurrence than the status of additional tumor bed margins, as stated by the authors.
The investigators aimed to identify the pathological factors associated with locoregional recurrence in patients with early-stage tongue squamous cell carcinoma who underwent surgery alone. Additionally, they explored the impact of a positive glossectomy specimen margin on disease control concerning final negative tumor bed margins.
The research included 110 patients diagnosed with pT1-2N0 oral tongue squamous cancer, adhering to the American Joint Committee on Cancer (AJCC) 8th edition criteria. These individuals underwent partial glossectomy and elective dissection from 2015 to 2021, excluding adjuvant radiation. Pathology reports were examined for factors such as tumor size, depth of invasion, glossectomy specimen margin, final tumor bed margin status, and perineural or lymphovascular space invasion. Individuals with positive final margins or a history of head and neck radiation were excluded.
The Kaplan-Meier method was employed to estimate locoregional control (LRC) and overall survival (OS), with a Cox proportional hazards model identifying prognostic factors for LRC in multivariate analysis.
Concerning baseline characteristics, the median age was 52 years, with the majority being male (54.5%) and having pT2 stage disease (58.2%). There were 33 lymph nodes dissected on average, and the median tumor size measured 16 mm, with a depth of invasion reaching 5 mm.
The majority of patients did not exhibit perineural invasion (84.7%), while 3.6% had lymphovascular space invasion. Positive glossectomy specimen margins were observed in 8.2% of cases.
Further findings revealed that among patients with positive glossectomy specimen margins and those without, the 3-year locoregional control (LRC) rates were 66.7% and 89.5%, respectively. Similarly, the rates were 0.0% for individuals with lymphovascular space invasion and 89.4% for those without. Among the 8 patients experiencing regional failure, 5 had recurrence in the ipsilateral neck alone (62.5%), 2 in the bilateral neck (25.0%), and 1 with isolated contralateral neck recurrence (12.5%).