There is great uncertainty among healthcare officials when considering the effects of increased hospital consolidation. Proponents of hospital mergers emphasize that such a refashioning of the industry will result in lower costs and greater efficiency. Skeptics of hospital mergers, grounding their argument in anti-trust rationale, believe that decreasing competition among hospitals will actually increase patient costs.
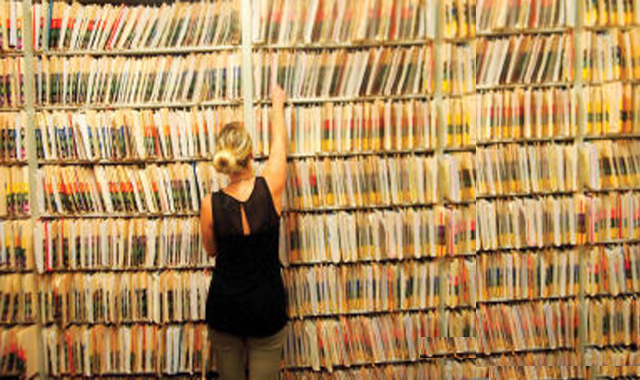
The Affordable Care Act (ACA) has no doubt been a catalyst for recent hospital merger activity as it provides incentives for reducing costs rather than rewarding volume of care. Uniting hospitals under common management reduces administrative costs, and advancing EMR technologies reduce risk and provide greater stability in the course of hospital network expansion. Health systems seek to expand their network because along with it comes a greater range of patient population-based knowledge and less risk in cost-effective decision making.
The range and scope of hospital mergers are far reaching. Definitive Healthcare has tracked 27 unique merger related stories just in the past month, including the $7.6 billion deal between Community Health Systems of Tennessee and Health Management Associates of Florida. Additionally, Definitive’s database evinces that two-thirds of hospitals are affiliated with a hospital network and the average size of a hospital network is just over seven hospitals. The prevalence of hospital mergers causes concern for both patients and insurers. In response, the Federal Trade Commission (FTC) has expressed serious attentiveness to hospital consolidation and the potential problems that it may pose.
Studies on the past hospital merger boom in the 1990s may perhaps lend some perspective on the influx of mergers catalyzed by the ACA. Robert Town’s empirical study, “The welfare consequences of hospital mergers,” concluded that hospital mergers in the 1990s caused a reduction in private insurance rolls and an increase in uninsured US residents but overall negligible welfare loss. Town cites numerous other reputable researchers that have also come to the conclusion that hospital mergers led to increased prices and effectively reduced consumer surplus by an estimated $42.2 billion between 1990 and 2001.
Empirical research drew the conclusion that even rival hospitals in the vicinity of merging hospitals experienced increased costs of care. Price increases are a result of increased hospital bargaining power, as merging reduces competition which in turn raises insurance premiums for patients. These mergers occurred while volume of care was still being rewarded of course. Despite these studies, health officials are confident that hospital mergers will lower costs and increase quality of care under the new guidelines of the ACA.
The American Hospital Association (AHA) conducted its own study and released a report in April of 2013 that addressed criticism of hospital consolidation. The report stressed that the majority of mergers involved the acquisition of a single hospital and that only 10 percent of community hospitals had been involved in a merger between 2007 and 2012. The AHA also emphasized the prevalence of hospital mergers among hospitals with less than 50 beds all in an effort to counter what the AHA believed to be sensationalized treatment of hospital merger related news.
It is difficult to draw conclusions about the overall impact of hospital consolidation due to the abundance of externalities and the uniqueness of the hospital market structure. In my previous article “Evaluating the first-year development of Pioneer ACO Model,” I had suggested that Pioneer ACOs with larger networks were more effective at generating savings than ACOs that were inferior in size. Hospital administrators are perhaps conscious of this trend and are actively engaging in a push to centralize management and patient information networks.
The overall end goal of the ACA is to transition to a population-based model of healthcare. Health systems that have a greater range of patient data will ultimately fare better because of the statistical advantages of making decisions in a larger patient population. Source