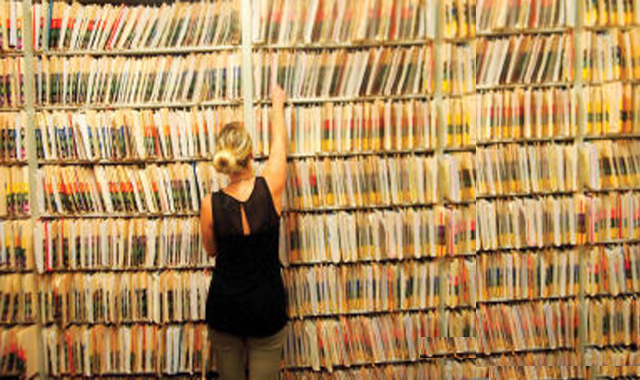
One pillar of this brave new world of health care is the idea that doctors, patients, insurers and other stakeholders will all have access to electronic health records.
Electronic health records, or EHRs, are such a central piece of reform that the government is helping to defray costs for hospitals and other health care providers to implement EHRs that meet federal standards. In 2009, the government passed the Health Information Technology for Economic and Clinical Health Act, which allows the Centers for Medicare & Medicaid Services to pay hospitals that meet “meaningful use” requirements.
In some ways, the incentives have been effective.
According to a study that the National Center for Health Statistics released earlier this month, 78 percent of office-based physicians used some kind of EHR in 2013, compared with 18 percent in 2001. Most office-based physicians thought EHRs were a good idea — 69 percent said they wanted to participate in the government’s “meaningful use” incentives. But only 13 percent of all office-based physicians both wanted to participate and have implemented systems that meet most of the government’s standards to receive meaningful use payments in 2014.
The uptake of EHRs matters to Nashville. First of all, a handful of local health care startups have business models that depend on access to EHR data, with the end goal of fine-tuning patient care. Secondly, meaningful use payments can be substantial. Nashville-based HCA, the nation’s most profitable hospital chain, took in $75 million worth of electronic health record incentive income during the third quarter of 2013. While companies do not expect these payments to be a major source of revenue forever, the bump never hurts.
If doctors tend to support EHRs and the money’s good, why wouldn’t everyone jump on this?
For one, EHRs can still be very expensive. When Franklin-based Community Health Systems introduced digital medical records at its hospitals, the incentive money wasn’t enough to offset lower patient volumes. The capital needed to meet meaningful use requirements is even more threatening to small, rural hospitals, said Mark Frisse, a professor of biomedical informatics at Vanderbilt University.
Vanderbilt has had an EHR system for more than 15 years. “The early users of EHRs were somewhat historical accidents,” said Frisse. “They were institutions where there were leaders with a strong vision for the importance of that. At Vanderbilt, this was clearly Dr. William W. Stead, who was the visionary who pushed this.”
Hospitals working on implementing EHRs are learning what Vanderbilt learned a long time ago — in addition to the short-term economic burden of going digital, it is really tough to make any change, no matter how needed, to a health care system.
A study published this month in the journal Medical Care surveyed 55 regional extension centers, which are organizations designed to help providers meet meaningful use requirements. In the study, these centers listed provider engagement and difficulty choosing an EHR system as the top two roadblocks preventing providers new to an EHR system from establishing one.
In other words, this is not a matter of building cutting-edge technology, it’s a matter of incorporating available tools into a system that only recently has had top-down incentives to do so.
The best way for providers new to these systems to move forward is to rip the Band-Aid off, suggests Dr. Farzad Mostashari, a co-author of the Medical Care paper. Once, he said, he and some colleagues attempted a piecemeal implementation of a type of EHR system.
“It turns out that pulling one little piece out and making this minimal change doesn’t work so well, …” he said. “So one of the lessons I’ve learned is don’t be afraid to take a plunge.” Source