Electronic medical records (EMRs) help both healthcare professionals and patients save time, improve care, and reduce expenses. But, like any rich well of data, there are plenty of organizations that want to mine this information for unrelated reasons.
There’s absolutely no reason to demand the unlikely return to manila folders and steel filing cabinets full of paper. There is, however, a need for healthcare IT executives to ensure patient data is protected, not only from hackers and careless employees, but from legitimate organizations that may benefit from what’s supposed to be privileged information.
Whether their motives are well meaning or financial, the result is the same: Giving organizations access to EMRs breaks the bond of confidentiality between patient and doctor. Once that’s broken, all the technological advances in the world won’t cut costs or improve health; patients may lie to doctors in order to avoid having a discoverable negative mark in their permanent medical record.
War on Drugs
Deaths from prescription drugs quadrupled between 1999 and 2010, according to an October 2013 report by Trust for America’s Help. In 2011, 6.1 million Americans abused prescription drugs, down from 7 million, the report found. Stronger laws, improved education, and accessibility to treatment programs got some of the credit — but obviously far too many people are still ensnared in the trap of addiction.
Currently, 49 states have a Prescription Drug Monitoring Program (PDMP) designed to help identify so-called doctor shoppers; problem prescribers (physicians), and people in need of treatment. The resources and use of these systems varies greatly by state, according to Trust for America, which wants to make sure PDMPs are integrated into EMRs “to quickly identify patients in need of treatment and connect them with appropriate care and identify doctor shoppers and problem prescribers.” That’s a laudable goal — unless this information also becomes accessible to law enforcement and, therefore, prosecution, cautions Dr. Adrian Gropper, who’s involved in the federal effort to link PDMPs to EMRs and to link these electronic patient records across state lines. He wrote:
Physician-patient confidentiality is important to public health, and networked electronic health records have both individual privacy and public health consequences. Privacy is essential in infectious disease testing, domestic violence, mental health, adolescent, reproductive, and addiction medicine. Subjecting clinical encounters to law enforcement surveillance beyond the physician’s discretion is life-threatening…
To my colleagues and public servants working to link prescription drug surveillance to medical records and health information exchange, I offer the following suggestion: let’s make the electronic health record a safe harbor from criminal prosecution. My health record should never be used as probable cause by law enforcement and it should never be given as evidence in criminal proceedings. The decriminalization of health records will underscore that drug abuse is a medical problem and it needs to be solved by medical professionals, not police, lawyers, and prisons.
Tragically, some people abuse prescription drugs. Some lie to doctors and fake symptoms for conditions they’re fortunate enough not to really have in order to take or sell the medications the doctor orders. But ceding privileged doctor-patient information to law enforcement in order to find criminal behavior, rather than using a subpoena to support an existing case, moves us closer to Orwell’s vision.
Big Pharma marketing
Investing in an EMR, especially now that government subsidies have expired, is an expensive proposition for medical offices. Instead of buying an on-site or hosted system, some healthcare providers are using free EMRs. That is, they come without an upfront charge, but developers support their software via advertising and crunching the data that comes from patient files, according Reuters.
Insurers use this deidentified data — that is, patient records stripped of names, according to Reuters (hopefully Social Security numbers, addresses, and other identifying info is also removed) — for multiple purposes, such as tracking flu outbreaks. Some EMR providers send pharmaceutical-funded vaccine reminders; PracticeFusion, for example, told Reuters it does not sell data to third parties, but analyzes the information within its internal cloud and then sells some of the results. These could be, for example, the number of adults within a region that have not yet had a particular vaccine.
Of course, most patients don’t know enough to ask about the type of EMR a doctor’s office uses. They’re not wondering whether information is housed by a vendor, whether it’s anonymized and sold, or whether it’s eyed only by staff. This “slippery slope” of data and EMRs is a problem, Dr. Adriane Fugh-Berman, director of PharmedOut, a research and education project at Georgetown University Medical Center, told Reuters. Patients often don’t know who is sending an email vaccine reminder or other content, which could be from the physician or an advertorial from a drug manufacturer, for example.
“It’s extremely misleading to patients,” Fugh-Berman said.
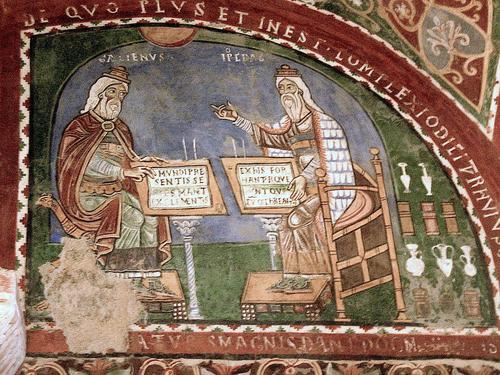
(Source: Wikipedia)
EMRs will expand until every physician in every specialty uses these interconnected systems — and that’s why it’s vital for the healthcare community to set the ground rules for patients’ privacy. “First, do no harm,” the Hippocratic Oath commands. Opening wide EMRs’ doors could do a lot of damage indeed. Source

























