Article Summary :
There seems to be an incorrect idea in the medical industry that it is okay to rip-n-replace existing EMR systems for reasons that don’t make sense. Hospitals waste millions when they rip out existing EMR systems and replace them and there is rarely a good reason. With numerous connectivity solutions, this former practice makes little sense. We would like to make the medical industry aware that this type of disruption is too costly and unnecessary.
Article in Detailed :
By Dr. Donald Voltz, MD, Aultman Hospital, Department of Anesthesiology, Medical Director of the Main Operating Room, Assistant Professor of Anesthesiology, Case Western Reserve University and Northeast Ohio Medical University.
A board-certified anesthesiologist, researcher, medical educator, and entrepreneur. With more than 15 years of experience in healthcare, Dr. Voltz has been involved with many facets of medicine. He has performed basic science and clinical research and has experience in the translation of ideas into viable medical systems and devices.
Thanh Tran, CEO of Zoeticx, Inc. also contributed.
A recent article (http://www.beckershospitalreview.com/healthcare-information-technology/why-we-switched-to-epic.html) has brought an example where a healthcare system has switched from an existing deployed EHR system to another one. Along with the effort, the healthcare system has also converted three outpatient facilities to one single vendor as well.
The decision to switch from one deployed system to another over concern of the vendor’s long-term prospect (support/maintenance/upgrade) is no doubt a justifiable one. However, ripping the whole infrastructure – inpatient and outpatient, in order to reach interoperability is certainly a questionable approach due to the cost, and the level of disruption to care providers. It should also be noted that disruption to care providers’ workflow is a direct correlation to a healthcare institute’s revenue and patient care quality.
From a technological standpoint, to be on the same database from the same vendor does not necessarily mean that interoperability is achieved. A recent data point from Epic on its own effort to showcase its interoperability support reveals that there are significant efforts required to even achieve Epic-to-Epic interoperability. http://www.hospitalemrandehr.com/2014/09/19/epic-wants-to-be-known-for-interoperability-are-they-interoperable/?utm_source=Healthcare+Scene&utm_medium=email&utm_campaign=af5c20c7c3-RSS_EMAIL_CAMPAIGN&utm_term=0_4092230e89-af5c20c7c3-61038365
These links indicate that Epic has made significant progress on Epic-to-Epic integration, but should both healthcare systems with the same software from the same vendor need any additional efforts for interoperability/integration? So the only way to reach interoperability is by using the same database model, as outlined from this article?
We believe that the reason for this is to address fragmentation of the software product. Fragmentation is a case where deployments from the same software product have gone through significant amounts of customization, leading to its divergence from the product baseline. Another high profile case of fragmentation leading to difficult integration and interoperability is the Department of Defense (DoD) and Veteran Administration (VA) with VistA.
Merger and acquisition trends in healthcare are ongoing. If we take the above scenario to one more level, what if the same healthcare system acquiring or being acquired takes the same approach–‘rip-n-replace’ again to reach interoperability. If integration strategy is simply based on rip-n-replace, and then rebuilding all the customized solutions again, what would it look like? What would be the cost? What would be the disruption level for care providers? How would the new healthcare system prevent patient care quality declining?
Other vertical industries have gone through the same cycle and the term ‘rip-n-replace’ has been a black mark in other IT industries. Even today, IT infrastructures still use mainframe computers because we cannot always ‘rip-n-replace’ in order to obtain integration and interoperability among software products. There are technologies which have proven effective in addressing integration in a heterogeneous environment. And healthcare as an industry is no different!
From a vendor perspective, there is always a push to remove its competitor’s products to increase market share. From the healthcare system perspective, this move represents cost, disruption of service and time to stabilize, including retraining staff for the new system.
In recent conference presentation, Dr. Donald Voltz on a similar topic ‘Less Disruption, Please!’ (https://www.youtube.com/watch?v=nd7bUVF_QW4) outlined the nature of what would be needed for interoperability from a physician’s stand point. We have enough disruption through our move from paper to electronic medical records. Continuous disruption in order to reach integration will have an even more severe impact to a healthcare institute’s operation and survivability.
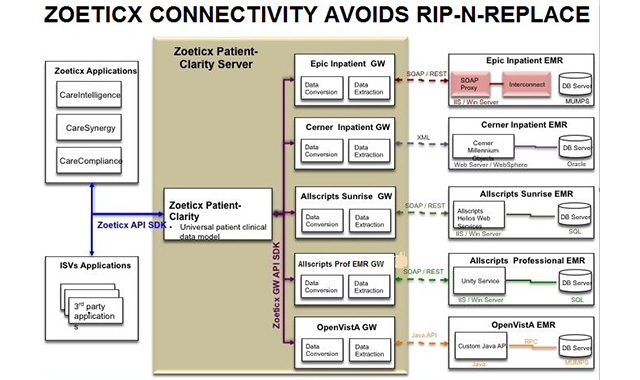
Service Oriented Architecture (SOA) is the technology stack supported by other vertical industries to address integration after decades of effort through other obsolete approaches such as EAI (Enterprise Application Integration). The Zoeticx approach is to take the same concept from SOA, make it applicable to healthcare (http://zoeticx.com/how-do-i-get-my-inter-campus-and-intra-campus-emr-healthcare-open-architecture-hoa/). HOA (Healthcare Oriented Architecture) leverages existing healthcare investments in EHRs and introduces less disruption to care providers through integration/interoperability efforts.