“Obamacare” may not please everybody, but Americans of all political stripes already benefit from at least one by-product of the new law: innovative health care technologies that make it easier and cheaper to access quality health care.
Accountable care requires that “hospitals defend the perimeter against avoidable admission,” said George Pace, a health care industry executive based in North Carolina. “If I’m there because of a heart attack, okay, but it’s not okay if it’s because I forgot to take my medications. You have to expand the continuum of care into the community and identify and address symptoms, illnesses, and behaviors before they escalate.”
That’s where technology comes in. Just as doctors and hospitals leverage “physician extenders” such as nurse practitioners and physician assistants to provide a broad range of services, said Pace, “technology extenders” such as mobile telemedicine, real-time collaborative tools and electronic monitoring systems will increasingly be used to maximize the reach of medical professionals, all while lowering costs.
In some rural communities, for example, local doctors have started to utilize remote presence devices — call them “robo-docs” — to teleconference with distant specialists as they examine patients. In the past, patients might have been forced to travel hundreds of miles at great expense to meet with specialists, or perhaps would have skipped the trip, only to land in the emergency room shortly thereafter.
Mark Twain Medical Center, a small, 25-bed hospital in San Andreas, California, recently acquired the RP-VITA, an advanced telemedicine robot from InTouch Health and iRobot (IRBT_). Outside medical specialists can direct RP-VITA, which looks a bit like R2D2 from Star Wars, only taller and with better posture, to a patient’s bedside to initiate a consultation or exam.
“We’re just beginning to realize telemedicine’s true potential in disease prevention,” writes InTouch Health on its corporate blog. “It doesn’t take a genius to understand that a 340-pound patient who doesn’t exercise or make regular primary care visits is a prime candidate for a stroke or heart attack. Telehealth e-visits and follow-ups can go a long way toward eliminating the need for remote stroke consultations down the road.”
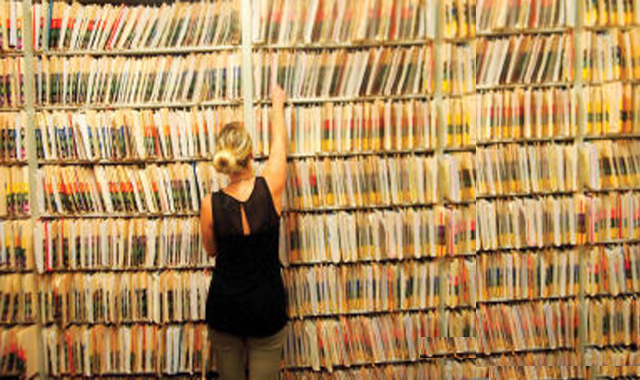
Accountable care also encourages health professionals across multiple disciplines and locations to collaborate on clinical care to avoid superfluous medical expenditures. Cooperation becomes even more vital as millions of newly insured patients — many with chronic conditions and little or no medical history — enter the health care system under the Affordable Care Act. That, said Pace, gives rise to a need for technologies that deliver personalized, real-time patient data into the hands of medical staff.
One such technology comes from AirStrip, whose AirStrip ONE health care mobility solution creates a “virtual bedside” by transmitting live, secure data from medical devices, patient monitors, and electronic medical records (EMR) to smartphones and tablets. AirStrip products initially covered obstetrics and in the last several years have expanded to include cardiology, patient monitoring and EMR.