Exclusive article at EMRIndustry
By Thanh Tran, CEO, Zoeticx, Inc.
Thanh Tran is CEO of Zoeticx, Inc., a medical software company located in San Jose, CA. He is a 20 year veteran of Silicon Valley’s IT industry and has held executive positions at many leading software companies. He is also a member of EMR Industries’ EMR Advisors.
Dr. John Loonsk’s recent blog, “Where’s the plan for interoperability?” poses a direct question on EHR Interoperability. Coming from the former ONC Director of Interoperability and Standards, the blog outlines the challenges towards healthcare interoperability:
- 1. Infinite extensible architecture
- 2. Discipline towards execution – “Interoperability is not about bright and shiny object solutions, it is about the much less glamorous work.”
- 3. EHR Silos and Standard Silos
- 4. Not focusing on the core challenges, i.e. patient engagement
- 5. HITECH and meaningful use focus must go beyond EHR vendors
The above five key points outline the challenges healthcare faces, in terms of deriving a national standard and reaping the benefit of the transition from paper to an electronic environment. Dr. Loonsk touched on the patient centric model as a critical missing link to any solutions presented today. In short, where is the patient – in the landscape of healthcare today?
From a patient centric perspective, we would like to offer a potential solution and roadmap in addressing healthcare interoperability:
- Patient-centric model: Any standard development must start with the patient. Addressing the patient needs would eventually align every other aspect required for interoperability. It is the patient who needs to have all of their clinical data connected and presented seamlessly to care providers.
- Focus on clinical data: Care providers ‘speak a universal language’ – it is the patient clinical data. Whether a heart rate can be stored under different files, different databases, or different electronic syntax to care providers, it is simply a heart rate. From a patient centric approach, the model is based on clinical data. To support healthcare, all vendors must adopt to the universal language for care providers.
- Open API /open architecture: With the patient-centric clinical data model, we support an open API / architecture and remove the healthcare applications required to operate on the data from the deployed EHRs’ infrastructure.
- Adopt a standard model and open API while leaving the task for translation to EHR vendors: Tightening the model and the API would force the issue of translation to a universal model. ONC should focus on tightening the rule with compliance to that model and leave EHR vendors with the task to do the conversion from its proprietary clinical data to the universal model.
- Patient directory services: Patient engagement would begin with the patients specifying which healthcare facility they would have their records hosted. The creation of a standard patient directory service would open accessibility and support of patient care continuum without the required data duplication as suggested in HIE. HIE is static in its approach, but a patient directory service with access via a gateway leaves the data at the source, ideal for healthcare! With this approach, EHR vendors would still have their stickiness in healthcare institutes, making them easier to adapt to a new model. At the same time, the patient directory service, coupling with the access approach at near time would give care providers the ability to retrieve the complete view of patient medical information.
This approach addresses most of the current shortcomings:
- Loose standard definition (CDA)
- Lack of focus entity (not patient centric)
- Incorrect emphasis from HITECH (EHR vendors) and an impractical approach for implementation due to additional components such as a centralized HIE database.
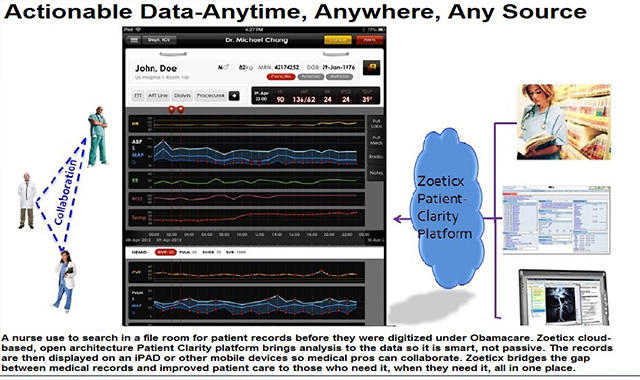
Our proposed solution is available through the Zoeticx approach which starts with focusing on the patient, clinical data and an open architecture to support near time access to EHRs.