Exclusive at EMRIndustry
By Thanh Tran, CEO, Zoeticx, Inc. and an EMR Industry Advisor
By Dave Streilein, CEO, Comprehensive Network Solutions Inc.
When Walter Cannon first identified homeostasis in 1930, he described how the human body maintains steady levels of temperature and other vital conditions. However, there was little thought to a health collaborative ecosystem. Healthcare has come a long way since then and homeostasis is now vastly different. Today, similar processes dynamically maintain steady-state conditions in the Earth’s environment. All care models and approaches must have their objectives on how to measure its outcome and for healthcare, it is all about patient outcome.
Reaching the State of Homeostasis as a Desired Patient Outcome
Homeostasis, a biological term, refers to the stability, balance, or equilibrium within a cell or the body. It is the process of maintaining a constant internal environment by providing the cells or body with what they need to survive (oxygen, nutrients, and removal of waste) for the well being of the cells or of the entire body. While disorders (physical or mental) reflect the abnormal condition of the body, homeostasis is the normal, stable and well-being state.
Healthcare’s objective is to improve patient care outcomes. A medical disorder is a deviation from the state of homeostasis. Each disorder is well documented with what would be a normal condition or simply put, the state of homeostasis. Homeostasis also deviates based on race, demographics, and above all, in its relationship with other existing disorders encountered by the patient and therefore can be noted that each patient outcome has a personalized state of homeostasis.
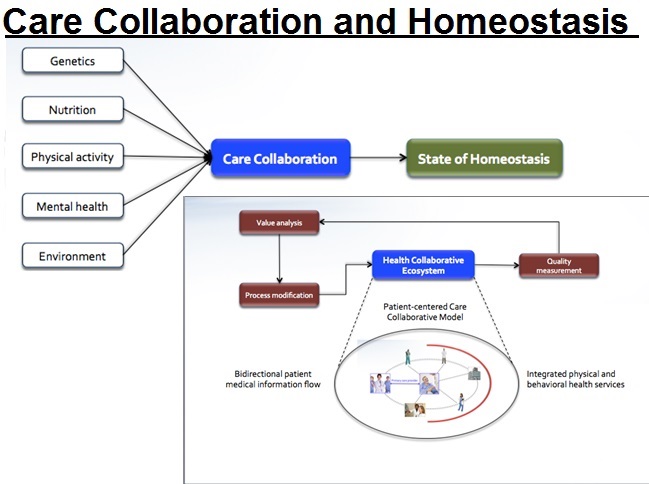
From the disorder, the process toward the state of homeostasis consists of genetics, nutrition, physical activity, mental health and external environment. Genetics is an internal influencer with medicine and physical care playing a role in adjusting the disorder towards a normal condition or homeostasis. For healthcare, it is the care plan for a disorder which could include a Patient-Centered Care Collaborative Model, the relationship between care collaboration and the state of homeostasis.
As disorders may have different processes to bring the patient back to the state of homeostasis, each of the processes require different care environments, supported by different specialists. Care collaboration is a requirement to effectively get the patient back to the state of homeostasis, and the state of homeostasis is the patient care outcome, supported by the care collaborative process covering all major elements in adjusting the patient’s well being back to the normal, equilibrium condition. The state of homeostasis should be used as the measure of a patient’s outcome, resulting from the care collaborative model addressing the integrated coordinated care from multiple care providers.
Health Collaborative Ecosystem
The Health Collaborative Ecosystem (HCE) is the delivery process supporting care collaborative model with the objective to bringing the patient to the state of homeostasis. This system would incorporate all providers of health-related services for the chronically ill patient diagnosed with one or more of the designated chronic and debilitating diagnosis that utilize the most significant percentage of health care spending. Such system would be:
- Capable of integrating physical and mental care environments.
- An integrated layer complementing (including EHR-agnostic) existing health IT infrastructure, supporting care activities beyond the brick and mortal walls of their facility or clinic.
- Consensus among providers to standards of care and bi-directional information flow that encourages innovation, compliance with regulations, secure privacy and adopts a continuous process of improvements to better reach patient state of homeostasis.
Why an Ecosystem?
An ecosystem is a collective system, including health IT solutions and consulting, guidance and support for a hospital’s operation in order to maximize the benefit of care collaboration through efficiency and scalability of care providers’ bandwidth. It is an ecosystem because it must include an audit and compliance component to provide crucial measurement and enforce quality guidelines for the model according to hospital clinic management. It is also an ecosystem because it must include the ability to track and monitor progress towards the state of homeostasis for all attributes contributing to the patient’s overall well being.
Case Scenario
Maria Viera, 75, takes a dozen medications to treat her diabetes, high blood pressure, congestion heart failure and arthritis. The situation worsens when her memory starts fading, leading her to forget about taking her medication. There are signs of depression developing as well. Additional concerned events such as hip and knee pain, dizziness, low blood sugar and a recent fall[1].
The care team for the above patient would potentially consists of a primary care provider (high blood pressure and care coordinator), a cardiologist (congestive heart failure), an endocrinologist (diabetes), dietician (diabetes), a rheumatologist (arthritis), physical and or occupational therapists (arthritis, falls, hip and knee pain), and a psychologist or a psychiatrist (depression). Today collaboration among the above care team members is done manually. The Health Collaborative Ecosystem perfectly fits the requirements to address all care needs and collaboration in order to bring the patient back to the state of homeostasis.
Net New Revenue Focusing On Preventive Care
The Health Collaborative Ecosystem is also the answer for the ‘revolving door care environment’ in addressing the need for integration between physical and behavioral health services. What is needed is a roadmap to roll out the Health Collaborative Ecosystem without upfront risks, budget planning and above all, the achievement of Net New Revenue for medical facilities. The implementation roadmap leverages the following CMS initiatives:
- Annual Wellness Visit
- Chronic Care Management
- Integration between physical and behavioral health through a care collaboration model
With the HCE objective for patient state of homeostasis, rural and community hospitals and clinics can accomplish multiple goals—better services to the community, better defined patient outcomes, opening of new avenues for health services with behavioral health and filling the revenue gap.
[1] Care Management Plus: Strengthening primary care for patient with multiple chronic conditions by Susan L Haydes and Douglas McCarthy