Exclusive at EMRIndustry.com
By Thanh Tran, CEO, Zoeticx, Inc. and an EMR Industry Advisor
By Dave Streilein, CEO, Comprehensive Network Solutions, Inc.
By David Conejo, CEO, Rehoboth McKinley Christian Health Care Services
(Part 1 of a 3 part series focusing on the health collaboration ecosystem and its ability to enable a patient to achieve a state of homeostasis.)
CMS (Center of Medicaid and Medicare Service) continues to increase emphasis on care collaboration, ranging from Chronic Care Management (CCM) to the recent announcement from the US Surgeon General’s landmark report on alcohol, drug and health. Derived from many aspects in healthcare, the authors’ examine the challenges of integrating physical and behavioral healthcare, addressing the Care Collaboration Model outlined by CMS and the Surgeon General.
In this second part of a three part series, the authors’ begin with the interdependency between physical and behavioral health, then introduce the care collaboration and provide case scenarios that outline the challenges of today healthcare.
Interdependency Between Mental and Other Chronic Disorders
A chart from the National Center for Chronic Disease Prevention and Health Promotion identifies the co-occurrence between depression and other common chronic conditions such as diabetes, cardiovascular, and cancer chronic conditions. Research has demonstrated bi-directional links between mental disorders and chronic conditions while depression and anxiety are heightening the risks towards hypertension and diabetes. Depression roughly doubles the risk for a new Coronary Heart Disease (CHD) event. A World Health Organization chart even goes further on other mental disorders such as PTSD, drug addiction and alcoholism.
Another study showed behavior health issues affecting patient recovery as follows:
- Cardiovascular – 23% affected
- Diabetes – 27% affected
- Cancer – 42% affected
- Parkinson – 51% affected
Such interdependencies have limited solutions today due to the lack of a collaborative environment. We refer to this situation as ‘revolving door care environment’, a vicious cycle compounding effects on chronic and mental disorders. A detox center can only retain the patient for detoxification. Without collaborating with other behavioral services, the patient would come back to the same habit – either drug addiction or alcoholism.
Such depression could be from social environment or from a recent developed chronic condition such as CHD. Primary care providers would continue to address the chronic condition without knowledge of what may actually feed into the patient chronic condition; another ‘revolving door’ for the physical care environment. In short, interdependency between mental and other chronic disorders must be addressed by the collaboration between physical and behavioral care services.
Care Collaborative Model and Bi-directional Information Flow
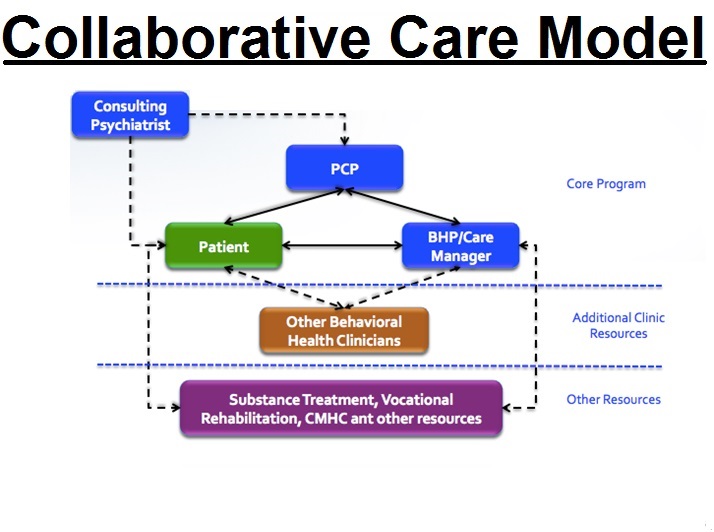
The Care Collaborative Model (CCM) is a multi-discipline approach to healthcare provided by care providers supporting and implementing treatment with the patient at the center. A bi-directional information flow is an absolute must to put the model into operation in healthcare institutes.
Currently, health IT identifies HIE (Health Information Exchange) as the basis of information flow between care providers; however, HIE flow is uni-directional as the information is “pushed” to the HIE by care providers. Other care providers “pull” the information without ongoing feedback or notification on an updated patient medical condition.
Without a bi-directional information flow, the CCM initiative cannot be put into operation. It should also be noted that this type of push and pull operation must be supported in an EHR-agnostic environment since healthcare institutes are deployed with EHR systems from multiple vendors.
Interoperability only addresses the challenge of accessing patient medical records. Such a challenge is referred, up to now, with solutions supporting a uni-directional information flow. A care collaborative model requires more than interoperability. It requires an environment where all care providers involved in patient treatment operate in sync.
Case Scenarios
As noted in one case study, Maria Viera, age 75, takes a dozen medications to treat her diabetes, high blood pressure, mild congestive heart failure, and arthritis. After she begins to have trouble remembering to take her pills, she and her husband visit her primary care physician to discuss this and a list of other worrisome developments, including hip and knee pain, dizziness, low blood sugar, and a recent fall. Maria’s primary care doctor spends as much time with her as he dares, knowing that every extra minute will put him further behind schedule. Yet despite his efforts, there is not enough time to address her myriad ailments. She sees several specialists, but no one talks to all her providers about her care, which means she may now be dealing with conflicting recommendations for treatment, or medications that could interact harmfully. As a result, Maria is at high risk for avoidable complications and potentially preventable emergency department visits and hospital stays.
This case study brings challenges to the health care system in multiple ways:
- More time from a primary care provider with limited results due to the lack of collaboration with other care providers, specialists and community services.
- Potential conflicting recommendations for treatment due to the lack of coordination and bi-directional medical information flows from multiple care providers and specialists.
- The patient risk for complications, emergency visits and hospital stays significantly increases.
- As a condition worsens, the patient develops symptoms for behavioral health conditions.
Today’s solution for the above scenario is to bring in the services of a care manager. It would be the care manager’s job to work with all care providers, manually “pulling and pushing” patient medical conditions and updates to all involved care providers. Error prone, high cost and low efficiency are some of today’s deficiencies for healthcare attempts in implementing and realizing a care collaborative model, as outlined by CMS.
Can Today’s Health IT System Support A Care Collaborative Model? If not, why?
EHR and EMR systems are the main ‘anchors’ of today’s health IT. Two EHR characteristics are non-starters. The first is limitations to the boundary of the health institute and uni-directional systems.
The second is the HIE (Health Information Exchange) that addresses EHR limitation with its capability to support cross health institutes, but actually further deepens the uni-directional character of EHRs. Patient medical data records are duplicated and consolidated for sharing purposes, but do not have a close loop feedback system to actively enable collaboration.
As this article focuses on the challenges in solving the interdependencies between physical and behavioral health, Part 2 will reveal the new disruptive concept in addressing CMS’s Care Collaborative Model with a well-defined patient outcome. In Part 3, the authors’ will also address how the new concept will result in better patient outcomes, net new revenue for healthcare systems and curbing the overall cost curve.