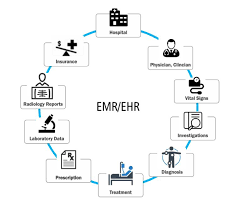
The electronic medical record (EMR) industry has experienced rapid growth, evolving from almost nonexistent in 2000 to a value exceeding $31 billion annually by 2018. Globally, EMR adoption is recognized as a vital step toward modernizing healthcare, aiming to enhance patient outcomes, improve health system efficiency, and unlock extensive research potential. The adoption of EMRs varies significantly based on each country’s socioeconomic policies, health system organization, financing, and the integration of primary and acute care networks. While high-income and upper-middle-income countries show varying degrees of EMR adoption, lower socioeconomic countries face challenges such as lack of funding and inadequate infrastructure, resulting in significantly lower adoption rates.
The impacts of EMR implementation on hospital business are diverse, encompassing improvements in quality, safety, information integrity, completeness, routine care integration, and data analytics for quality improvements and research. However, these impacts, while valuable, often do not yield immediate financial returns and are challenging to quantify, leading them to be excluded from traditional financial-based business cases for EMR investment.
A recent attempt to synthesize research and empirical evidence by Lau and Kuziemsky aimed to provide guidelines for identifying and measuring the benefits of digital health implementation. The framework focuses on measuring successful Information and Communications Technology (ICT) implementation and identifies three eHealth benefit domains: care quality, access to care, and productivity. Economic methods applicable for eHealth benefit evaluation were briefly discussed, informed by a scoping review of 33 economic evaluation studies applied for Health Information Systems (HIS) between 2000 and 2013.
Despite governments providing incentives and subsidies for EMR adoption due to perceived benefits and the infrastructure nature of EMR, the cost-effectiveness of this investment has been questioned. This is partly attributed to providers making token attempts to meet meaningful use criteria without capturing the economic values of EMR investments.
The variety of EMR implementations in both acute and primary care settings adds complexity to evaluating their economic impacts. As resource and fiscal constraints become more prominent, there is a growing need for robust conceptual frameworks to systematically identify, measure, and value the economic impacts of EMR investments.
The project’s objective is to contribute by exploring existing options in academic literature and practical applications for evaluating the economic worth of EMR.
It seeks to develop a cost-benefit analysis framework to identify, measure, and value the impacts of EMR in the Australian hospital-care setting. The initial step involves a comprehensive scoping review examining how EMR implementations in the hospital setting have been evaluated using cost-benefit analysis approaches internationally.
In the initial phase, the scoping review extensively explored both peer-reviewed and gray literature to acquire a thorough understanding of the evaluation methods, economic advantages, and associated costs linked to the implementation of Electronic Medical Records (EMR) in hospital settings. Significantly, the focus was specifically directed at EMR systems operating within hospital contexts, deliberately excluding those deployed in primary care or non-hospital settings. The exploration centered around key research questions:
Q1: The investigation aimed to ascertain the number of studies qualifying as full Cost-Benefit Analyses (CBA) in comparison to partial economic analyses. Special attention was given to evaluating whether these studies engaged in comprehensive discussions on benefits and costs, considering diverse stakeholder groups and analytical perspectives.
Q2: The analysis delved into the composition of benefit or cost items, scrutinizing whether they had a financial or economic nature. The inquiry extended to understanding the methods used for measurement and valuation, while also uncovering key assumptions or findings related to changes over time and across different settings.
Q3: The investigation concentrated on extracting primary findings related to net impacts, such as net benefits or net costs. Additionally, efforts were made to determine whether the literature provided explanations for the observed impacts, aligning with the quadruple aims of healthcare delivery.
Within the context of this review, a CBA study was defined as one involving the identification, measurement, and comparison of the benefits and costs of an EMR implementation program or project. These costs and benefits were expected to be presented quantitatively, utilizing financial and/or economic data and summarized through metrics such as net present values (NPVs), internal rates of return (IRRs), or returns on investment (ROIs). Studies calculating net financial cost or incremental cost-effectiveness ratio (ICER) were not excluded but were not classified as CBAs. The analyses were anticipated to reflect an assessment of opportunity costs, acknowledging the trade-off of resource allocation for EMR projects against alternative healthcare endeavors.
The subsequent stages of the scoping review, spanning from inclusion criteria and search strategy to data extraction and collation of findings, adhered to rigorous methodologies in alignment with established guidelines such as PRISMA. The overarching objective of this comprehensive process was to synthesize varied findings from the literature, offering nuanced insights into the economic dimensions of EMR implementation in hospital settings.