By Dr. Donald Voltz and Eric Tran, Master of Science in Microbiology and Immunology, School of Medicine, Tulane University, New Orleans, LA.
The COVID-19 virus is ravaging the planet at a scale not seen since the infamous Spanish Flu of the early 1900s, inflicting immense devastation as the U.S. loses more than 200,000 lives and counting. According to CDC statistics, 94% of patient mortalities associated with COVID-19 were simultaneously suffering from preexisting conditions, leaving a mere 6% of victims with COVID-19 as their sole cause of death. However, while immediate prospects for a mass vaccine might not be until 2021, there is some hope.
The fact that four in ten U.S. adults have two or more chronic conditions indicates that our most vulnerable members of the population are also the ones at the greatest risk of succumbing to the pandemic. Healthcare providers must pay close attention to patients harboring 1 of 13 chronic conditions believed to play major roles in COVID-19 mortality, particularly chronic kidney disease, hypertension, diabetes, and COPD.
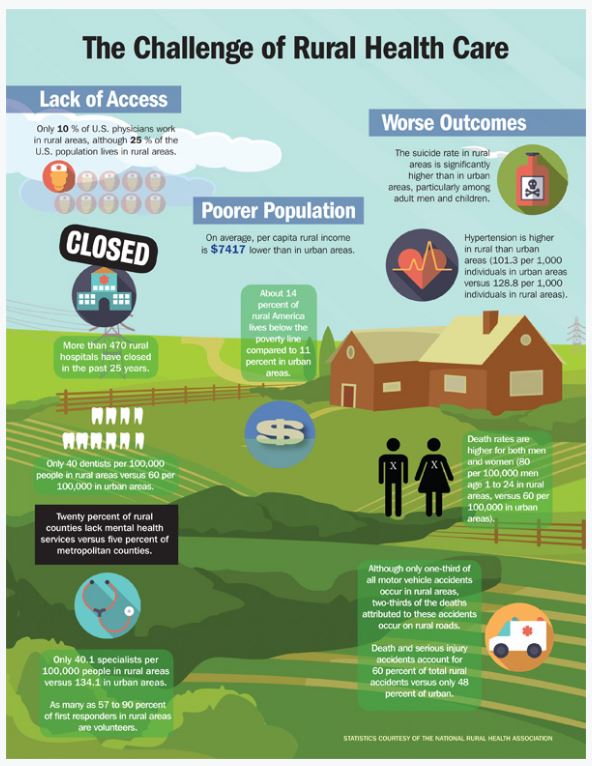
Rural populations are some of the most vulnerable and must be supervised due to their unique challenges. The CDC indicates 80% of older adults in remote regions have at least one chronic disease with 77% having at least two chronic diseases, significantly increasing COVID-19 mortality rates compared to their urban counterparts.
Health behaviors also play a role in rural patients who have decreased access to healthy food and physical activity while simultaneously suffering high incidences of smoking. These lifestyle choices compound with one another, leading to increased obesity, hypertension, and many other chronic illnesses. Overall, rural patients that fall ill to COVID-19 are more likely to suffer worsened prognosis compared to urban hubs, a problem only bolstered by their inability to properly access healthcare.
COVID-19 has shown the cracks in the U.S. healthcare system that must be addressed for the future. Even if COVID-19 were to fade away on its own, the next pandemic may not. Furthermore, seasonal influenza serves as a reminder that healthcare is not a skirmish, but a prolonged war against disease. Rather than doom future generations to suffer the same plight our generation has with the pandemic, now is the time to develop innovative strategies that focus on protecting our most vulnerable citizens by leveraging existing healthcare initiatives to focus on proactive responses instead of reactive responses.
On the Right Road
While some of the most vulnerable people are the elderly, rural residents and the poor, the good news for them is that CMS have long advocated the use of preventive care initiatives such as Chronic Care Management (CCM) and Remote Physiologic Monitoring (RPM) to track these geriatric patients. To encourage innovation in this sector, CMS preventive care initiatives provide generous financial incentives to healthcare providers willing to shift from conventional reactive care strategies to a more proactive approach focused on prevention and protection.
These factors led to the creation of numerous patient CCM programs, allowing healthcare providers to remotely track the health status of geriatric patients suffering from numerous chronic conditions. The tracking is at a rate and scope unseen previously through the use of electronic media. Interestingly enough, the patients already being monitored by CCM programs overlap heavily with populations susceptible to COVID-19. To adapt existing infrastructure for the COVID-19 pandemic is a relatively simple task.
One growing CCM program that could be retrofitted to deal with the COVID-19 pandemic are the use of telehealth services in rural locations. Prior to the pandemic, telehealth services were one of the many strategies advocated by the CDC to address the overtaxed healthcare systems found in rural locations.
The reason for the CDC’s interest in telehealth was that telehealth meetings could outright remove the need for patients to travel and allow healthcare providers to monitor patients at a fraction of the time. By simply coupling existing telehealth services with CMS preventive care initiatives focused on COVID-19, rural healthcare providers could detect early warning signs of COVID-19.
This integration at a faster and far greater scale could mean much greater preemptive virus detection through routine telehealth meetings. The effect of telehealth would be twofold on both rural and urban health communities. It could slow the spread of COVID-19 to a crawl due to decreased patient travel and improved patient prognosis through early and intensive treatment for vulnerable populations with two or more chronic health conditions.
This integrated combination would shift standard reactive care to patient infections to a new monitoring methodology that proactively seeks out infected patients and rapidly administers treatment to those most at risk of mortality. This new combination of preventive care and telehealth services would not only improve patient and community health, but would relieve the financial burden incurred from the pandemic due to the existing CMS initiatives subsidizing such undertakings.
In conclusion, preventative care targeting patients with pre-conditions in rural locations are severely lacking in the context of the COVID-19 pandemic. By leveraging CMS preventive care initiatives along with telehealth services, healthcare providers can achieve the following care objectives.
First, there are financial incentives with preventive care services that will relieve the burden on healthcare systems. Second, COVID-19 vulnerable populations will receive the attention and focus from healthcare providers that they deserve to slow the spread through the use of early detection systems and alerts to their primary health provider. Third, by combining with telehealth service, healthcare providers can efficiently and effectively reach out to rural populations that were once inaccessible to standard healthcare practices.